Cataract Surgery and the Vestibular Patient: A Call for Increased Awareness and Collaboration
While cataract surgery is a successful procedure for vision restoration, it presents unique and unexpected challenges for patients with vestibular disorders. As vestibular rehabilitation specialists, it is crucial to recognize these specific challenges and take proactive steps to minimize complications.
The Crucial Role of Vision in Balance
It's important to emphasize that clear vision is essential for balance, especially in individuals with vestibular impairments. Improving gaze stability and visual acuity can significantly enhance balance function and reduce fall risk—however, the type of vision correction matters.
The Interplay of Vision and Vestibular Function
The visual and vestibular systems are intricately linked, working synergistically to maintain spatial orientation and postural control. When the vestibular system is compromised, the central nervous system often increases its reliance on visual cues for balance. While beneficial in many circumstances, this adaptive mechanism can become problematic in cataract surgery, particularly with multifocal IOLs.
The sudden influx of clear visual information following cataract surgery can create a sensory mismatch, as the brain struggles to integrate the new visual input with the existing vestibular information. This mismatch can manifest as dizziness, imbalance, and visual vertigo, especially in individuals with pre-existing vestibular deficits.
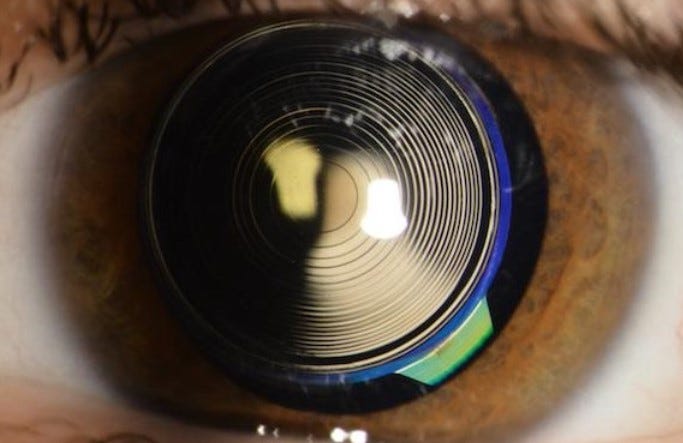
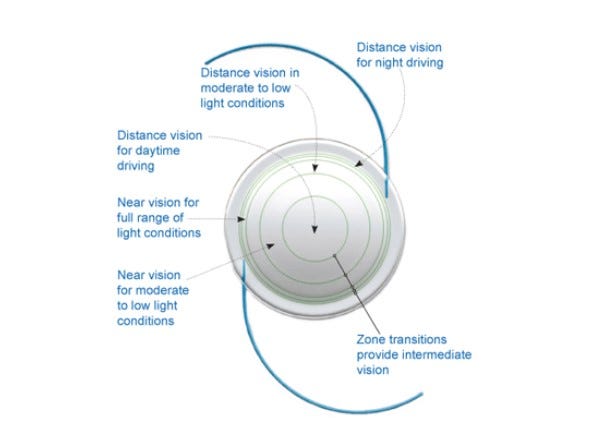
Multifocal Lenses: A Cause for Concern
The increasing popularity of multifocal intraocular lenses (IOLs) further complicates the visual-vestibular interaction in post-cataract patients. While these lenses offer the advantage of reduced dependence on glasses, they present a unique challenge to the brain's visual information processing.
Multifocal IOLs create multiple simultaneous images on the retina, requiring the brain to selectively filter and interpret the appropriate focal point for a given distance. This increased visual complexity can overwhelm the already challenged vestibular system, exacerbating dizziness and imbalance symptoms.
This is particularly concerning for patients with:
Pre-existing vestibular disorders: Including vestibular migraine, post-concussion syndrome, bilateral or unilateral vestibular hypofunction, and recurrent BPPV (which can indicate underlying utricular dysfunction and affect the linear vestibulo-ocular reflex).
Migraine history: Migraines can significantly impact visual processing and sensory integration.
Judy's Story: A Cautionary Tale
Judy, a 56-year-old female, came to our clinic with severe dizziness following cataract surgery. She had opted for multifocal lenses to address both near and far vision. However, the surgery triggered a cascade of debilitating symptoms, including constant dizziness, a feeling of falling, and severe motion sickness.
Further assessment revealed that Judy had underlying vestibular impairments, including vestibular migraine and central oculomotor instabilities. Unfortunately, her pre-existing vestibular dysfunction was not identified before surgery, and the multifocal lenses exacerbated her condition to the point where she ultimately required further surgery to have them replaced with mono-focal lenses.
Judy's story highlights the critical need for:
Thorough pre-surgical screening: Including a detailed history of dizziness and balance problems and vestibular assessments when indicated.
Careful consideration of lens choice is essential, especially for patients with any history of vestibular migraine symptoms of findings.
Early intervention: Prompt referral to vestibular rehabilitation for patients experiencing persistent dizziness after cataract surgery.
Optimizing Vestibular Function through Prehabilitation
Prehabilitation is key to mitigating the risk of post-surgical vestibular complications. Before cataract surgery, vestibular rehabilitation specialists should:
Thoroughly assess vestibular function: Identify any pre-existing deficits that may increase the risk of post-surgical complications.
Implement a targeted prehab program: This should include vestibular balance exercises to enhance vestibular function and reduce reliance on visual cues for balance.
Educate patients on potential risks: Discuss the possibility of dizziness and imbalance following cataract surgery, particularly with multifocal IOLs.
Collaborate with ophthalmologists: Advocate for a multidisciplinary approach to patient care, ensuring open communication and shared decision-making regarding lens selection and post-surgical management.
Early Intervention is Crucial for Post-Surgical Dizziness
Physicians should proactively identify patients who exhibit persistent dizziness post-surgery, particularly around week 3 or 4 when initial healing is typically complete, and promptly refer them to vestibular rehabilitation. This timeframe allows for adequate tissue healing while ensuring timely intervention to address the visual-vestibular mismatch and optimize recovery.
Vestibular rehabilitation is crucial in facilitating adaptation to the altered visual environment. Interventions may include:
Habituation exercises: Reduce sensitivity to visual motion and conflict.
Gaze stabilization exercises: Improve visual fixation and reduce oscillopsia.
Balance training: Enhance postural stability and reduce fall risk.
Sensory strategy analysis and therapies: Recalibrate sensory systems and optimize sensory re-weighting.
Patient education: Provide strategies for managing symptoms.
The longer a patient waits to address post-surgical dizziness, the more challenging it can be to achieve optimal recovery.
Conclusion
While beneficial for visual acuity, cataract surgery can present significant challenges for patients with vestibular disorders. By understanding the intricate interplay between the visual and vestibular systems and implementing proactive pre-surgical prehab and comprehensive post-surgical management strategies, vestibular rehabilitation specialists can be vital in optimizing patient outcomes and minimizing the risk of postoperative complications.
A collaborative approach between ophthalmologists and vestibular therapists is not just beneficial; it's essential. This approach ensures that patients receive comprehensive care and achieve optimal functional recovery following cataract surgery, making us all part of a team working towards a common goal.