Dynamic Visual Acuity Testing: A Cornerstone of Vestibular Assessment

Dynamic Visual Acuity (DVA) testing is a cornerstone of vestibular assessment, offering critical insights into a patient's ability to maintain clear vision during head movement. However, there's often confusion surrounding its proper execution and interpretation. This in-depth guide aims to clarify the nuances of DVA testing, dispel common misconceptions, and equip vestibular professionals with the knowledge to perform and interpret this valuable assessment accurately.
The Essence of DVA Testing
DVA testing evaluates the vestibulo-ocular reflex (VOR), a fundamental mechanism stabilizing our gaze during head movements. A robust VOR ensures that the world remains clear even when our heads are in motion, allowing us to navigate our environment effectively. DVA testing quantifies the effectiveness of this reflex by measuring how much visual acuity decreases during head movement.
Dispelling the ‘First Line Deficit’ Myth
A common misconception is to focus solely on the first line where a patient exhibits a deficit during head movement. This approach overlooks the critical importance of comparing dynamic visual acuity to static visual acuity (SVA), which is the patient's visual acuity with their head still. The accurate measure of DVA lies in the difference between SVA and DVA, often termed ‘lines lost.’ This difference reflects the impact of head movement on visual clarity and provides valuable information about the integrity of the VOR.
The Gold Standard Methodology
Establish SVA: Begin by assessing the patient's best-corrected visual acuity with their head stationary. This provides the essential baseline for comparison. Use a standardized eye chart, such as the ETDRS chart, ensuring proper lighting and viewing distance.
Measure DVA: Instruct the patient to oscillate their head horizontally at a consistent speed while reading the eye chart. Identify the lowest line they can read clearly during this movement. To standardize head movement:
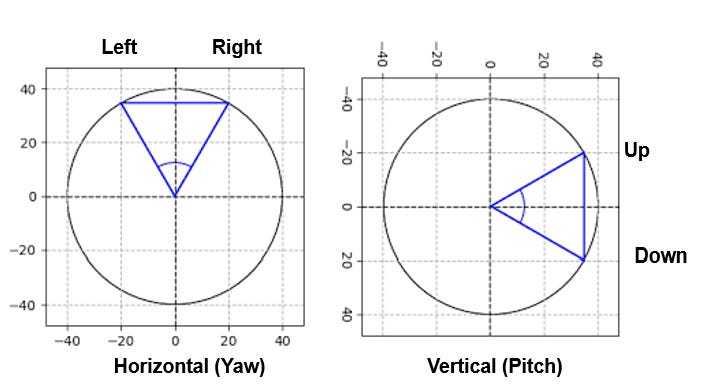
Head Velocity: Aim for a peak head velocity (PHV) of approximately 120 degrees per second. This velocity can be achieved by maintaining a head movement arc of about 40 degrees (Horizontal - 20 degrees to the right and 20 degrees to the left—Vertical - 20 degrees up and 20 degrees down).
Using a Metronome: A metronome can help patients maintain a consistent head movement speed. Setting the metronome to 120 beats per minute allows for two cycles of head movement per beat, or 240 beats per minute allows for one cycle of head movement per beat.
Passive Head Movement: Ensure that head movement is passive, meaning the examiner gently moves the patient's head. This passive movement ensures a consistent velocity and prevents the patient from slowing down or stopping when the letters become blurry, which can lead to inaccurate results.
Calculate ‘Lines Lost’: Subtract the DVA line number from the SVA line number. This difference reflects the degree of VOR impairment. For example, if the patient can read line 11 with their head still (SVA) but only line 7 with head movement (DVA), they have lost 4 lines of acuity.
Why ‘Lines Lost’ Matters
The number of lines lost provides critical information about the severity of the VOR deficit. Here's a general guideline, illustrated with some examples:
Mild Deficit (1-3 lines lost): A 10-year-old child with dizziness and difficulty copying notes from the whiteboard might exhibit a 2-line loss, indicating a mild VOR deficit that could be contributing to their academic challenges. This might manifest as difficulty keeping their place while reading or copying notes, and they might experience dizziness or headaches after school.
Moderate Deficit (4-6 lines lost): A 45-year-old individual with BPPV experiencing dizziness when reaching overhead might show a 4-line loss, suggesting a moderate deficit that could impact their daily activities. This person might have difficulty with activities like driving, grocery shopping, or playing sports, and they may experience nausea or vomiting in addition to dizziness.
Considerable Deficit (7-9 lines lost): A 60-year-old patient with Meniere's disease might present with a 7-line loss, reflecting a substantial deficit and the disease's significant impact on vestibular function. This individual may experience frequent episodes of vertigo, hearing loss, tinnitus, and difficulty maintaining balance in challenging environments.
Severe Deficit (10 or more lines lost): A 70-year-old individual with a history of strokes and significant balance difficulties might be unable to read any lines on the chart during head movement. This indicates a severe VOR impairment and the need for ongoing support. The person may require assistive mobility devices and experience significant limitations in daily activities.
DVA and Bilateral Vestibular Hypofunction
While the above examples illustrate general DVA deficits, it's essential to consider how DVA findings relate to bilateral vestibular loss:
7-9 Lines Lost: This range often suggests bilateral vestibular hypofunction, especially when combined with symptoms like oscillopsia (the illusion of objects moving), difficulty with balance in low-light conditions, and a history of ototoxic medication use or conditions affecting both inner ears.
10 or More Lines Lost: This degree of loss strongly indicates significant bilateral vestibular impairment. Individuals in this category often experience severe oscillopsia and significant balance challenges and may require assistive devices for mobility.
Expanding to Vertical DVA
While horizontal DVA testing is standard, assessing vertical DVA is equally essential. Vertical VOR deficits can contribute to symptoms like dizziness and imbalance when looking up or down, climbing stairs, or navigating uneven terrain. Incorporating vertical DVA testing into your assessment provides a more comprehensive understanding of VOR function in all planes of movement.
Conclusion
Both horizontal and vertical DVA testing are indispensable parts of vestibular assessment. By adhering to the correct methodology and interpreting the "lines lost" accurately, we gain valuable insights into VOR function and can tailor effective rehabilitation programs to improve our patients' balance, stability, and quality of life.