Flying Blind: Beyond Desensitization and Habituation in Vestibular Rehabilitation - Part 2: How's He Flying Now?

As a physical therapist specializing in vestibular and balance disorders and the National Director of Vestibular Education & Training at FYZICAL, I've always been struck by the fascinating parallels between flight and balance. Both demand a complex interplay of sensory information, precise motor control, and unwavering trust in one's instruments, whether in the cockpit or the human body. This trust in our internal 'instruments' is not just crucial; it's the foundation of our practice. Just as a pilot undergoes rigorous training to master instrument flight, we, too, must guide our patients to trust in their 'instruments' as they navigate the often-challenging terrain of balance rehabilitation.
In vestibular rehabilitation, we often work in a 'blind' environment, especially when using virtual reality (VR). This controlled 'blindness' is a powerful tool. It allows us to move beyond simply habituating patients to challenging stimuli and facilitates faithful adaptation – effectively 'taming the lion' of their disrupted balance system.
My patient, Pete, a former instrument-rated pilot, provided a unique opportunity to explore these parallels in depth. His understanding of flight dynamics and the critical difference between visual and instrument flight proved invaluable in his rehabilitation journey. Pete and I spoke yesterday, and he has permitted me to share his test results with you - thank you, Pete.
Let's break down the nuances one more time:
Visual Flight vs. Instrument Flight:
Visual Flight: This method relies on visual cues – the horizon, landmarks, etc. – to maintain orientation and control. It's intuitive and how most people learn to fly initially. However, it's unreliable in poor visibility or when visual cues are misleading.
Instrument Flight: Relying on instruments – altimeter, airspeed indicator, artificial horizon – to provide accurate information about the aircraft's position and attitude, regardless of external visibility. It requires training, trust in the instruments, and disregarding potentially conflicting visual information.
The Vestibular System: Our Internal 'Instrument Panel'
The vestibular system in the inner ear is our body's 'instrument panel' for balance. It provides crucial information about head position and movement in space, working in concert with visual and somatosensory (touch and proprioception) input.
Vestibular Disorders: 'Flying Blind'
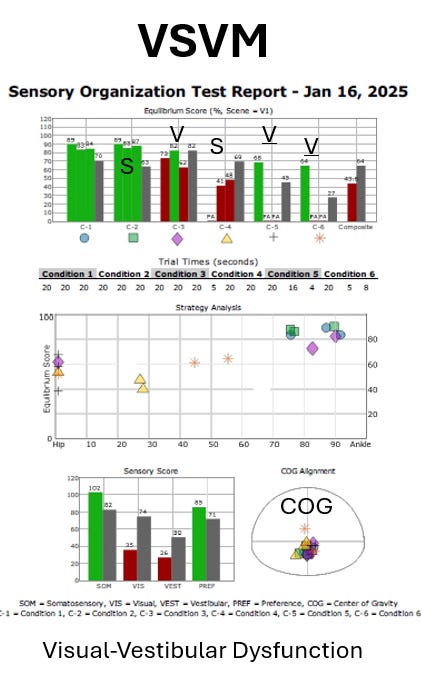
When the vestibular system malfunctions, it's like experiencing an 'instrument failure.' The brain receives inaccurate or conflicting information, leading to a range of debilitating symptoms, including dizziness, vertigo, and imbalance. Just like a vision-trained pilot caught in a cloud bank, patients with vestibular disorders can become overly reliant on visual cues, leading to a dangerous cycle of visual dependency (VVM). In some cases, patients may over-rely on surface cues (SVM) or a combination of both (SVVM or VSVM).
VR: 'Instrument Training' for Balance
This is where VR shines as a tool in the clinic. By immersing patients in a virtual environment and carefully manipulating visual input, we can effectively simulate 'instrument conditions' for balance. These conditions mimic the reliance on instruments in instrument flight, forcing patients to rely more on their somatosensory and vestibular systems, much like instrument-rated pilots rely on their instruments.
Beyond Desensitization: Adaptation and Neuroplasticity
VR allows us to go beyond traditional habituation exercises. We're not simply trying to reduce sensitivity to visual motion; we're actively retraining the brain to process sensory information more effectively. The controlled optic flow within the VR environment becomes a powerful tool for neuroplasticity, driving adaptation and promoting a more balanced reliance on all sensory systems. We are 'taming the lion’ of their imbalance.
Pete's Case: A Pilot's Perspective
Pete's background as an instrument-rated pilot gave him a unique advantage in understanding and engaging with VR therapy. When visual information was unreliable, he understood the importance of trusting his 'internal instruments' – his somatosensory and, more importantly, vestibular systems. This connection facilitated his progress and reinforced the power of VR in vestibular rehabilitation.
Expanding on Pete's Journey: Continued Progress and Persistent Challenges
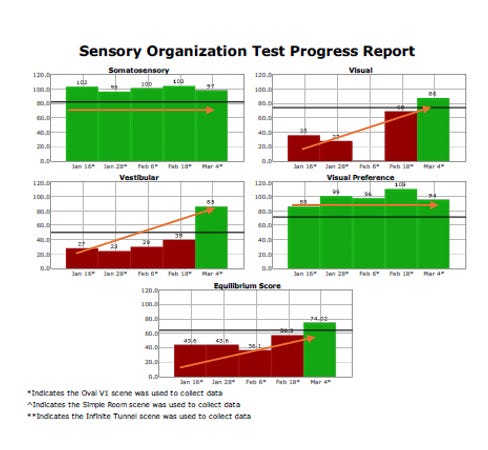
Building on the foundation of Pete's initial rehabilitation, we've witnessed remarkable progress, mirroring the transition from visual to instrument flight. As detailed above, Pete's background as an instrument-rated pilot provided a unique advantage in understanding and navigating the complexities of vestibular rehabilitation. His ability to grasp the concept of relying on internal 'instruments' when external cues were unreliable proved invaluable. This progress is a testament to the potential of VR in vestibular rehabilitation and should encourage us all in our practice.
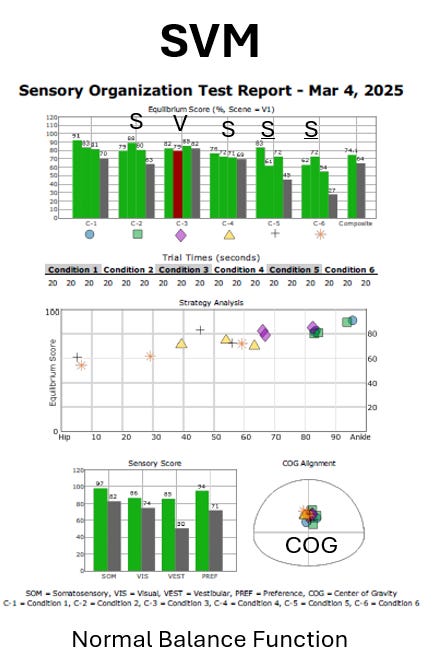
Since the initial phase, Pete has demonstrated significant objective improvements. His balance testing reflects a more integrated sensory strategy, a clear shift from the initial visual and surface dependency (VSVM). This improvement is tangible, as evidenced by his increased stability and confidence in various environments. However, like a pilot encountering unexpected turbulence, Pete's journey is not without challenges. These challenges, including specific turbulence in his rehabilitation journey, can provide valuable insights into the complexities of vestibular rehabilitation.
One of the inherent challenges in vestibular rehabilitation is differentiating between habituation and adaptation, particularly when applying disrupted sensory inputs. Consider using an unstable surface, such as a foam cushion. Is the cushion's effect merely passive—a consistent but unchanging stimulus the patient habituates to over time? In this scenario, repetitive exposure might lead to a habituated response, where the patient's symptoms decrease, but the underlying sensory processing deficit remains unchanged.
Using an irregular surface, such as foam, disrupts somatosensory inputs, forcing the central nervous system to adapt by using more visual and vestibular inputs. This approach is more neuroplastic and likely long-term.
In contrast, true adaptation involves neuroplastic changes within the central nervous system, leading to a more permanent and functional improvement in sensory integration. In Pete's case, we are aiming for adaptation.
We can consider these concepts through the lens of 'bottom-up' and 'top-down' approaches. The unstable surface represents a 'bottom-up' approach, where the disruption originates from the somatosensory system, driving changes in higher-level processing. Optokinetic flow within VR goggles can exemplify the 'top-down' approach. Here, the visual system is manipulated, influencing how the brain processes vestibular and somatosensory information. Understanding and applying these approaches can significantly enhance the effectiveness of vestibular rehabilitation.
Like a passive foam surface, optokinetic flow could be a habituation exercise. It involves passive exposure to a noxious or abnormal stimulus, which changes symptoms and potential signs. Remember that dizziness has signs and symptoms. The signs of dizziness are eye and body imbalance (e.g., static and dynamic, orthopedic). The symptoms are how the patient feels. Often, habituation stems more from how the patient feels, but it can potentially reduce the signs.
However, the impairment sign I believe we're seeing is more associated with the adaptation occurring. The brain is disengaging from the visual conflict and forcing itself to become stable and symptom-free by increasing somatosensory and vestibular integration—thus, 'flying by instruments.' We strive for this in therapy: to facilitate true adaptation and a more resilient, integrated balance system.
Despite the substantial progress, Pete continues to exhibit a degree of surface dependency (SVM - Sensory Mismatch). This means he still relies too heavily on somatosensory cues, particularly when visual or vestibular information is compromised. While his overall balance has improved, this lingering dependency can manifest as subtle instability, especially on uneven surfaces or in situations requiring rapid postural adjustments.
We've intensified Pete's exercise program to address this, focusing on activities that challenge his reliance on surface cues. We're incorporating dynamic movements, varied surfaces and head positions, and controlled visual distractions to refine his sensory integration further. These exercises push him beyond his comfort zone, promoting neuroplasticity and fostering a more balanced reliance on all sensory systems.
Furthermore, we continue to emphasize the importance of trusting his 'internal instruments.' Just as a pilot must learn to disregard conflicting visual information and trust their instruments, Pete is learning to trust his somatosensory and vestibular systems, even when they may initially feel unreliable.
The analogy of instrument flight remains a powerful tool in Pete's rehabilitation. By understanding the critical difference between relying on external cues and trusting internal feedback, he's actively participating in his recovery, 'taming the lion' of his imbalance and regaining his confidence and stability. We will continue to progress his exercises and monitor his progress.
The Future of VR in Vestibular Therapy
VR holds immense potential for transforming how we approach and treat vestibular disorders. It allows us to create personalized, engaging, and challenging experiences that push patients beyond their comfort zones and promote actual neuroplastic change. By embracing the principles of instrument flight, we can empower patients to regain their balance, confidence, and freedom.
Key Takeaways for Physical Therapists:
Acknowledge the inherent risks: VR therapy, especially in the early stages, can be disorienting and potentially dangerous. Prioritize patient safety at all times.
Understand the distinction between visual and instrument flight: This analogy can help patients grasp the concept of visual dependency and the need to retrain their brains.
Embrace VR as a tool for 'instrument training' for balance: VR allows us to create controlled environments that challenge patients and promote neuroplasticity.
Go beyond desensitization: Use VR to drive adaptation and re-integrate sensory information. We are "taming the lion" of their imbalance.
Empower patients: Help them understand their condition and actively participate in their recovery.
By thoughtfully integrating VR and 'instrument flight' principles into our clinical practice, we can help patients like Pete "fly" again, navigating their world with renewed confidence and stability.
References
Vestibular therapy: An Approach to Concussion, Strokes, and More. https://www.orlandochiropracticneurology.com/post/vestibular-therapy-an-approach-to-concussion-strokes-and-more