Inhibitory Cutoff: The Hidden Limit in Vestibular Function – Why It Matters for Your Balance and Vision - Part 1 of a 2-Part Series

As physical therapists specializing in vestibular and balance disorders, we constantly strive to understand the intricate mechanisms that govern our patients' symptoms. One crucial, yet often overlooked, physiological phenomenon is the Inhibitory Cutoff (IC). This concept is fundamental to grasping why some patients struggle with balance and vision, even after significant recovery from a vestibular event.
The Vestibular System and the VOR: A Quick Refresher
Our inner ear is home to the remarkable vestibular system, a complex and often unsung hero of balance and spatial orientation. It perfectly harmonizes with our eyes and somatosensory cues to keep us upright and maintain clear vision. Understanding the intricacies of this system is a lifelong journey for us as healthcare professionals, underscoring the depth of our knowledge and the crucial role we play in understanding and treating vestibular disorders.
The VOR, a key player in maintaining our balance and clear vision, is a lightning-fast reflex that stabilizes our gaze. When you turn your head, your eyes move in the opposite direction, keeping your vision steady. This reflex is incredibly rapid, with a latency of just 5-6 milliseconds, preventing the visual blur known as oscillopsia. Understanding the VOR's role in these functions is not only important, but also crucial to understanding the impact of IC on balance and vision, and thus on patient care.
What Exactly is Inhibitory Cutoff?
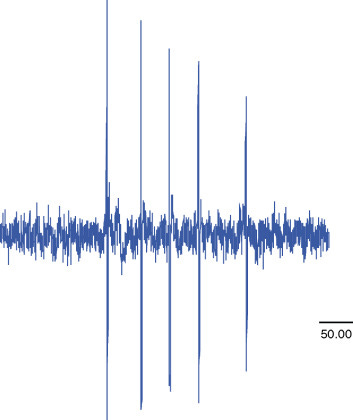
Vestibular neurons have a baseline firing rate. When your head moves, this rate either increases (excitation) or decreases (inhibition). The inhibitory cutoff is a hard physiological limit: a vestibular neuron's firing rate cannot drop below zero.
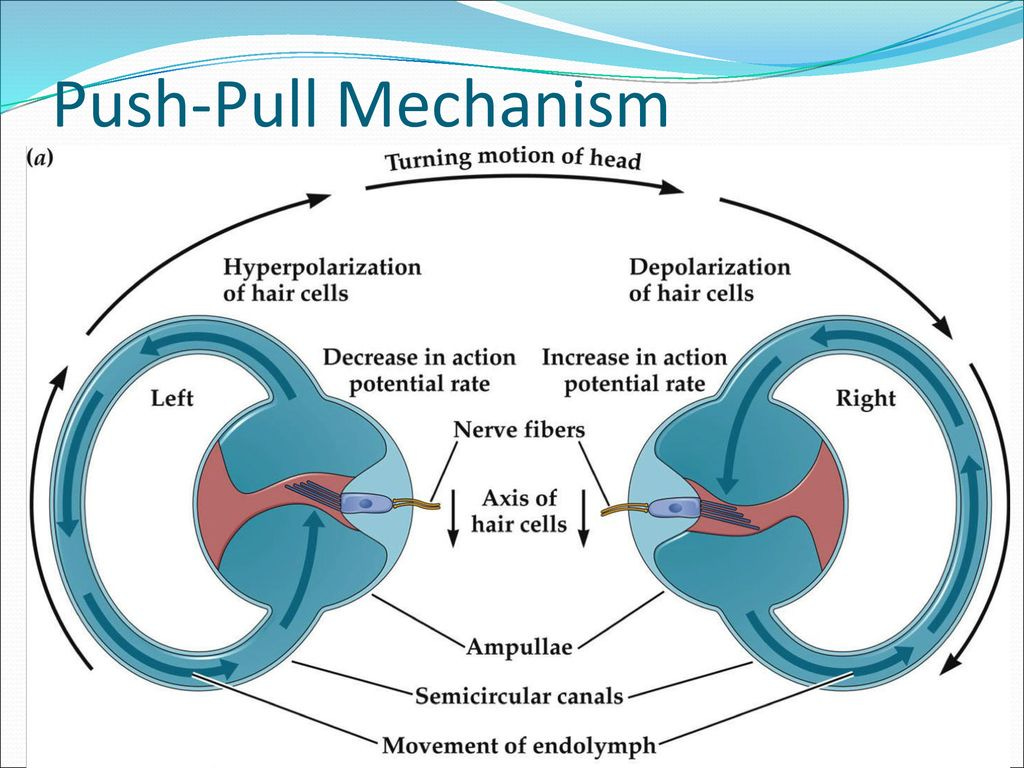
Think of it like this: your semicircular canals work in 'push-pull' pairs. A head turn to the right excites the right canal and inhibits the left, creating a balanced signal to your brain. However, if you make a very rapid head movement (typically involving accelerations of 2000-6000 degrees per second squared), the inhibitory signal to one canal can be so strong that its firing rate hits zero, disrupting this 'push-pull' balance.
When this cutoff occurs, that side can no longer provide its 'pull' signal. This results in an asymmetric message to the brain, even in a healthy system, at extreme velocities. This disruption is particularly significant for the phasic components of the VOR, which are responsible for our rapid, initial eye movements. Interestingly, these components are not just susceptible to IC; they are the most adaptable pathways for central compensation after a vestibular injury, making understanding IC even more crucial.
Inhibitory Cutoff in Unilateral Vestibular Hypofunction (UVH)
In conditions like vestibular neuritis, where one inner ear is damaged (Unilateral Vestibular Hypofunction or UVH), the impact of IC becomes even more pronounced. The natural push-pull mechanism is already compromised.
Turning towards the lesioned side: The damaged canal cannot generate a sufficient excitatory signal when you turn your head towards the affected ear. This directly leads to a significantly diminished VOR gain, as the "push" from that side is weak or absent. This is often the most obvious deficit.
CRUCIAL TO UNDERSTAND: Turning away from the lesioned side (towards the intact side): This is where a vital nuance of Inhibitory Cutoff comes into play. When you turn your head towards the intact ear, the healthy canal on that side is typically excited and fires. However, the vestibular system relies on a balanced ‘push-pull’ signal from both ears to accurately convey head velocity. The lesioned side, which should be providing a reciprocal inhibitory signal (a ‘pull’ to complement the intact side's ‘push’), is compromised. Because its baseline firing rate is already low or absent due to the hypofunction, it cannot provide the necessary, robust reciprocal inhibition.
This lack of effective inhibition from the lesioned side means the brain isn't receiving the complete, symmetrical information it expects. At high head velocities, this imbalance can effectively ‘force’ the intact side's neurons into a relative state of Inhibitory Cutoff within the overall system's context. While the intact side still provides a strong excitatory signal, the overall VOR response diminishes because the brain cannot perfectly interpret the head velocity without the complementary inhibitory signal from the lesioned side.
This also leads to a diminished VOR response in this direction, though often less severely than when turning towards the lesioned side. This subtle deficit is critical because the overall system's asymmetry at high speeds can affect even the "good" ear's contribution.
The result is a persistent VOR asymmetry, especially during high-frequency, high-acceleration head movements. While central compensation can help restore symmetry for slow, low-frequency movements, the effects of Inhibitory Cutoff at high frequencies often remain. This highlights the importance of ongoing patient care and underscores our role in delivering it.
Diagnosing the Invisible: Key Vestibular Tests
Because IC primarily affects high-frequency responses, specialized tests are not just important; they are crucial to unmask these deficits and ensure accurate diagnosis:
Video Head Impulse Test (vHIT): Our go-to for assessing VOR function across all six canals at high accelerations (100-250°/s). It directly reveals reduced VOR gain on the affected side and the presence of corrective saccades (eye movements that "catch up" to the target). A VOR gain below 0.8 is generally considered pathological.
Caloric Testing: While a gold standard for detecting unilateral weakness, caloric tests operate at low, unphysiological frequencies. A regular caloric test does not rule out a high-frequency VOR deficit related to IC.
Rotary Chair Testing (Velocity Step): This test measures VOR over a broader frequency range. High-velocity rotations (e.g., 180-240°/s) are powerful enough to induce Inhibitory Cutoff, helping us understand the individual contribution of each ear. It's the gold standard for diagnosing bilateral vestibular loss.
Combining these tests provides a comprehensive picture of vestibular function across different frequency domains, essential for accurate diagnosis.
Understanding the Head Impulse Test: What to Look For
When performing a head impulse test (manually or with vHIT), understanding the expected eye movements is crucial for identifying a vestibular hypofunction. This test helps us observe the VOR's ability to stabilize the eyes during quick head movements.
Let's consider a patient like Robert, a 52-year-old male. Last month, he experienced a severe episode of vertigo that landed him in the emergency room, where he was unfortunately discharged with a vague diagnosis of ‘dizziness.’ His primary care physician, knowing our expertise, referred him to FYZICAL for vestibular rehabilitation. As you take his history, you strongly suspect a unilateral hypofunction, possibly associated with a recent viral infection. Now, you're ready to perform the head impulse test, and this is what you're looking for:
A positive head impulse test indicates a peripheral vestibular hypofunction on the side the head is turned towards when the corrective saccade is observed. For Robert, if you perform a rapid head impulse to the right and observe her eyes drifting with her head, followed by a quick ‘catch-up’ saccade, this would strongly suggest a right-sided vestibular hypofunction. Conversely, if the same finding occurs with impulses to the left, it points to a left-sided issue. A negative head impulse test means the VOR is intact for that canal, and the eyes remain stable on the target without corrective saccades. This understanding helps us precisely pinpoint the affected side and confirm our suspicions, moving beyond a general ‘dizziness’ diagnosis to targeted intervention.
The Clinical Impact: When Balance and Vision Fail
An impaired VOR, particularly when impacted by Inhibitory Cutoff, leads to a range of disabling symptoms. These 'invisible' symptoms, which include dizziness, vertigo, imbalance, oscillopsia, and gaze instability, profoundly impact quality of life.
Dizziness and Vertigo: Sensations of disorientation or spinning.
Imbalance: Difficulty with walking, standing, and overall unsteadiness.
Oscillopsia: The distressing sensation of objects bouncing or jiggling during head movements, making tasks like reading or driving incredibly difficult.
Gaze Instability: The inability to maintain a stable focus during head motion, leading to blurred vision.
They can lead to reduced independence, increased fall risk, anxiety, depression, and cognitive issues like 'brain fog.' Objective tests, such as vHIT, are vital for validating these subjective complaints and understanding the full extent of the impact of vestibular disorders on patients' lives.
Furthermore, understanding VOR patterns from vHIT is crucial for differentiating between peripheral (e.g., vestibular neuritis) and central (e.g., stroke) vestibular disorders. For instance, a PICA infarct often shows normal VOR gain bilaterally, contrasting sharply with the unilateral loss seen in peripheral lesions. This distinction is paramount for guiding appropriate and timely treatment.
Conclusion: Why Understanding IC is Essential for Patients Like Sandra
Inhibitory Cutoff is a fundamental physiological limit that significantly impacts vestibular function, especially in patients with unilateral vestibular hypofunction. While the brain is remarkably adaptive, it cannot fully overcome the hard ceiling imposed by IC at high velocities. The brain's adaptability is genuinely awe-inspiring. For patients like Robert, whose initial "dizziness" masked an actual vestibular deficit, understanding IC is paramount.
As clinicians, recognizing the role of Inhibitory Cutoff allows us to:
Diagnose vestibular disorders with greater precision: Moving beyond vague diagnoses to pinpoint the specific nature of the problem, as we would for Sandra's suspected unilateral hypofunction.
Manage patient expectations about recovery: Acknowledging that while significant improvement is possible, some high-frequency challenges may persist due to the inherent physiological limits of IC.
Tailor rehabilitation strategies: Addressing specific, frequency-dependent deficits, often incorporating substitution strategies alongside adaptation to help patients like Robert navigate dynamic environments more effectively.
Improve patient quality of life: By validating their often ‘invisible’ symptoms and guiding effective treatment. Understanding why she feels unsteady during quick head turns, even if her balance seems better at rest, can be incredibly empowering for Sandra.
A holistic, multidisciplinary approach that considers both the physical and psychological aspects of vestibular disorders is not only important but essential for truly empowering our patients. As healthcare professionals, we play a crucial role in this approach.