The Dix-Hallpike Test: When Up Isn't Down and Right Isn't Left

As vestibular professionals, we are intimately familiar with the Dix-Hallpike Test (DHT) and its role in diagnosing Benign Paroxysmal Positional Vertigo (BPPV). But do we need a crucial piece of the puzzle when interpreting the results and choosing the proper treatment?
The Case of the Confusing Nystagmus
Picture this: your patient and you perform a DHT to the right, exhibiting the classic upbeat, rightward torsional nystagmus. Our instinct might be to immediately diagnose the right posterior canal BPPV and perform an Epley maneuver. However, this nystagmus could be deceptive, masking a different underlying cause.
The Inhibitory Factor and Neural Tension
While excitatory nystagmus from the right posterior canal is a common culprit, we must also consider the possibility of inhibitory nystagmus originating from the left anterior semicircular canal (ASC). This isn't just a mechanical phenomenon; it's also about the neural connections between these canals.
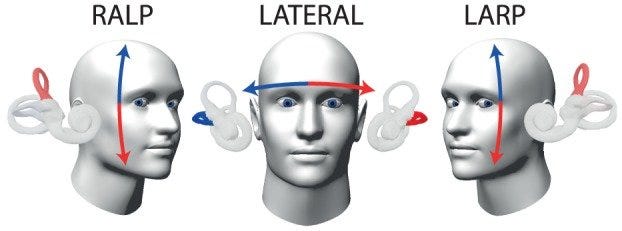
The LARP Plane: The right posterior canal (PSC) and the left ASC are paired in a functional plane known as the LARP (Left Anterior, Right Posterior) plane. These canals have a push-pull relationship, meaning that the excitation of one leads to the inhibition of the other.
Neural Tension: In our scenario, the correct PSC, through excitation, creates a neural "tension" that results in upbeat and rightward torsional nystagmus. Similarly, the left ASC, through inhibition, also contributes to the upbeat and rightward torsional nystagmus due to the decreased firing rate interpreted as relative excitation of the correct PSC.
Two Canals, One Nystagmus
This scenario highlights a crucial point: two different canals can generate the same nystagmus through distinct mechanisms. The right posterior canal (excitation) and the left anterior canal (inhibition) can contribute to the upbeat, rightward torsional nystagmus, reflecting the underlying neural tension within the LARP plane.
Diagnostic Considerations
This complexity demands a more nuanced approach to BPPV diagnosis:
Thorough History: Don't just focus on the nystagmus. Obtain a detailed history, including symptom triggers and characteristics.
Keen Observation: Pay close attention to subtle variations in nystagmus, which may provide clues about the involved canal(s).
Comprehensive Testing: Utilize a variety of positional tests to assess all three semicircular canals.
Targeted Treatment: The Key to Success
Accurate diagnosis is only the first step. The key to successful BPPV management is appropriately treating the right canal. This targeted approach ensures effective treatment and instills confidence in both patient and clinician.
Posterior Canal (PC) BPPV: If the correct PSC is confirmed as the culprit, both the Epley and Semont maneuvers are viable options.
Epley: A gentler, sequential maneuver that guides otoconia back to the utricle.
Semont: A quicker, more forceful maneuver that dislodges otoconia. The choice depends on patient comfort, clinician preference, and BPPV characteristics.
Anterior Canal (AC) BPPV: If the left ASC is the source of the problem, simply sitting the patient upright often does the trick. Gravity helps dislodge the otoconia from the canal, reducing inhibition and restoring balance. To further encourage the otoconia to return to the utricle, have the patient perform a gentle head nod while sitting upright. This can help ensure complete resolution of the vertigo. In some cases, additional maneuvers like the head-hanging or liberatory maneuver may be necessary further to facilitate the movement of otoconia out of the canal.
The Takeaway
By recognizing the potential for inhibitory nystagmus, the involvement of multiple canals, the neural interplay within the LARP plane, and the need for targeted treatment, we can refine our diagnostic skills and improve patient outcomes. Let's embrace the complexity of the vestibular system and strive for a deeper understanding of BPPV.
Let's discuss it! Have you encountered cases where the nystagmus didn't match the expected canal involvement? Share your experiences and insights in the comments below. Your contributions will enrich our knowledge and foster community and collaboration among vestibular professionals.