The Dizzying Deception: When BPPV Throws You a Curveball

Imagine a patient with a classic BPPV presentation walking into your clinic. They describe the familiar 'Roll over in bed, instant vertigo' scenario. You think, 'Easy case, posterior canal, Dix-Hallpike, done.' But then, the unexpected happens. Instead of the anticipated upbeating torsional nystagmus, a fierce right-beating horizontal nystagmus erupts. Your clinical radar screams: 'Horizontal canal!' A quick roll to the left reveals a less intense left-beating nystagmus. Suddenly, you're not in Kansas anymore. This isn't your standard BPPV case; you've stumbled into the geotropic maze of horizontal canal BPPV, and it's time to pull out your vestibular detective hat.
Understanding the Horizontal Canal:
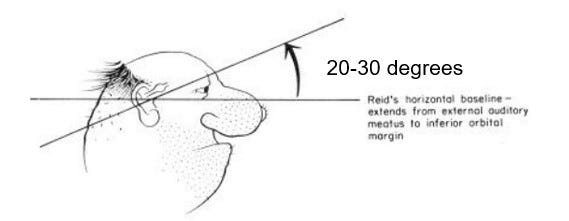
Unlike the other canals, the horizontal semicircular canal is roughly horizontally in the head (20-30 degrees off the transverse plane called Reid's line).
This seemingly simple fact leads to a complex presentation. The canal can be divided into the short arm (connected to the utricle and ampulla) and the long arm. The long arm further subdivides into the anterior (ampullary) and posterior (non-ampullary) segments. In geotropic horizontal BPPV, the debris resides in the posterior segment – a crucial detail for effective treatment.
The Diagnostic Dilemma: Supine Head Roll Test and Sidelying:
The supine head roll test is our primary tool for diagnosing horizontal BPPV. To perform it correctly, in supine, the patient's head must be flexed 30 degrees to align the horizontal canals perpendicular to the ground. This ensures an accurate assessment, avoiding weakened responses due to the canal's natural angulation.
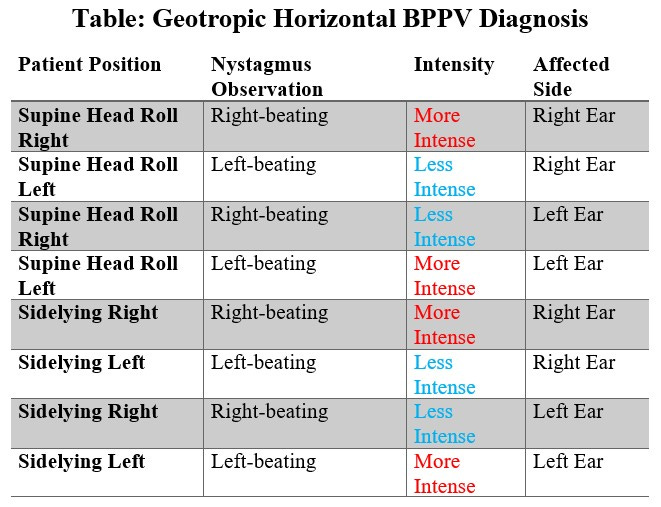
The challenge arises when interpreting the nystagmus. Geotropic nystagmus presents with a beat toward the ground on the affected side. Remember, the side with the more intense nystagmus and symptoms during the head roll or sidelying test is the affected ear.
Example: If the patient experiences more intense right-beating nystagmus when rolled to the right (i.e., positional nystagmus), the right ear is likely the culprit. Why this is happening is for another talk, but remember, it's all about the orientation of the hair cells.
If the supine head roll test is not an option, sidelying can be used. Again, pay close attention to which side elicits the more intense nystagmus (follow the signs).
Determining the Affected Side: Geotropic Horizontal BPPV
"To help clarify the diagnostic process, here's a table summarizing the key findings in geotropic horizontal BPPV:"
Table: Geotropic Horizontal BPPV Diagnosis (if listening, review the table when you get a chance)
The Effective Solution: The Gufoni (Appiani) Maneuver:
"Once the affected ear is identified, the Gufoni (Appiani) maneuver, named after its true originator, Gufoni, becomes our primary treatment strategy. It's crucial to understand the anatomy to avoid exacerbating symptoms.
Key Point: Treating geotropic horizontal BPPV incorrectly can lead to severe nausea and vomiting and even convert the condition to apogeotropic BPPV.
Here's the step-by-step procedure:
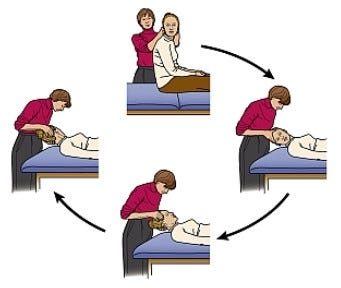
Short Sitting: Begin with the patient sitting on the edge of the treatment table.
Identifying the Affected Side: As we mentioned, the side that produced the most intense nystagmus is the affected side. In this case, let’s say it was the right side.
Lying Down (Unaffected Side First): If we determined the right side was affected, you would lie the patient down on their left side. This position moves the debris away from the ampulla, producing an inhibitory nystagmus (left-beating).
Wait until the nystagmus and symptoms subside, typically 1-2 minutes.
Head Turn (45 Degrees Down): Turn the patient's head 45 degrees nose-down towards the table. Hold for another minute. This allows the debris to fall directly into the utricle.
Sitting Up: Bring the patient directly up to sitting, maintaining the nose-down position. Observe for any residual nystagmus. If none is present, the maneuver was successful."
Avoiding Common Pitfalls:
A common mistake is treating the affected side directly, which can worsen symptoms. Understanding the canal anatomy and the physics of debris movement is essential for effective treatment.
Treating the GEO HSC-BPPV toward the affected side first will cause the debris to move towards the ampulla twice, causing a severe excitatory response, which is the opposite of what you want. In my beginning years as a therapist, particularly with canal switches after an Epley maneuver, I would convert to a GEO HSC-BPPV. I would inadvertently cause severe nausea and vomiting by rolling the patient the wrong way, leading to an ultimate conversion to an APO HSC-BPPV.
Key Concept: Treat TOWARD the unaffected side first to move the debris away from the ampulla."
Conclusion:
"Mastering the diagnosis and treatment of horizontal geotropic BPPV requires a deep understanding of vestibular anatomy and physiology. Adhering to the correct procedures and avoiding common pitfalls can alleviate our patients' symptoms and improve their quality of life.
This is a complex topic, and I encourage you to continue seeking advanced vestibular rehabilitation education. At FYZICAL, we are committed to providing the highest quality education and training to empower clinicians in this specialized field. We also use the SOS system at FYZICAL to ensure patient safety during these maneuvers. We can provide the best care for our patients by staying updated with the latest advancements.
Call to Action:
Have you encountered challenges with horizontal BPPV? Share your experiences and questions in the comments below! Your insights can contribute to our collective understanding and improve patient care. Subscribe to my Substack for more insights into vestibular rehabilitation. Check out FYZICAL's education courses for more in-depth training.