The Rhythmic Trap Tightens: Expanding on Entorhinal Entrainment and Visual Recalibration in MdDS

This article builds upon my previous exploration of visual strategies for Mal de Debarquement Syndrome (MdDS), specifically how Optokinetic (OPK) stimulation can influence the translational VOR. Here, I delve deeper into another compelling theory that may further illuminate the persistent symptoms of MdDS: the entrainment of the entorhinal cortex. Understanding how rhythmic motion can imprint itself on this brain region is crucial, as it may provide a more comprehensive framework for our visually driven therapeutic interventions.
The Brain's Unwitting Synchronization: Entorhinal Entrainment in the Genesis of MdDS
Entrainment, a fundamental principle in neuroscience, describes the synchronization of rhythmic neural activity with an external rhythmic stimulus. Think of a marching band: if one section starts playing at a particular tempo, others will naturally fall into that same rhythm over time. Similarly, in the context of MdDS, the repetitive motion experienced during travel – the very trigger I suspect of influencing the linear vestibular system – may also affect the entorhinal cortex. This central hub of spatial information processing, located within the temporal lobe and boasting extensive connections throughout the brain, including areas crucial for sensory processing, memory, and even emotional processing areas like the amygdala, plays a pivotal role in perceiving and navigating our environment.
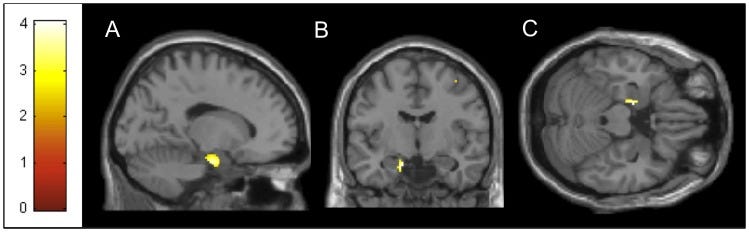
My theory suggests that the rhythmic bobbing, swaying, or rolling of a boat, the consistent vibrations of an airplane, or the predictable undulations of a train can, over time, entrain the inherent firing patterns of neurons within the entorhinal cortex. This synchronization disrupts the normal flow of communication between the entorhinal cortex and its vast network of connections, potentially leading to widespread neural oversynchronization. Intriguingly, PET imaging studies have revealed areas of relative hypermetabolism within the entorhinal cortex of individuals with MdDS, lending empirical support to this theory of central nervous system involvement.
The Lingering Echo: Entorhinal Entrainment and the Persistence of Symptoms
The concept of entrainment may also provide a crucial piece in the puzzle of why MdDS symptoms can be so persistent, often outlasting the initial trigger by weeks, months, or even years. Once the rhythmic activity within the entorhinal cortex becomes synchronized with the external motion, this new neural firing pattern may become ingrained within brain circuits. This persistent entrainment could explain why the sensation of motion continues even without any actual movement, as the brain's internal rhythm is now attuned to a moving baseline.
Furthermore, the entorhinal cortex's significant role in memory consolidation during sleep might explain the frequently reported delayed onset or exacerbation of MdDS symptoms after rest. During sleep, the entorhinal cortex actively communicates with the hippocampus, a key region for learning and memory, potentially solidifying the entrained rhythmic activity within neural networks. This consolidation process could lead to a more pronounced manifestation of MdDS symptoms upon waking, as the brain fully transitions back to processing the external, stable environment through this altered internal rhythm.
Visual Recalibration as an Anti-Entrainment Strategy
Our visually driven recalibration strategies for MdDS, utilizing OPK stimulation, may directly target this entrained rhythmic activity within the entorhinal cortex and broader brain networks.
Our OPK protocols, employing controlled linear and rotary visual flow, introduce a new, deliberately constructed visual rhythm. I hypothesize that this controlled sensory input, by engaging the visual pathways and their extensive connections with the vestibular system and the entorhinal cortex, can act as a counter-rhythm to the maladaptively entrained neural firing. By presenting a consistent and often opposing visual 'motion' while the patient remains physically stable, I am providing a novel sensory reality for the brain to process.
The neuroplasticity I aim to induce through carefully titrated OPK therapy, combined with balance retraining, could involve actively disrupting this pathological entrainment. The brain, constantly working to resolve the conflict between the perceived visual motion and the body's actual stillness, may begin desynchronizing the previously established rhythmic patterns within the entorhinal cortex and other interconnected areas. The active engagement and focused attention required during these visual exercises may further facilitate this "untraining" process.
A Unified Perspective: Towards More Effective Treatment and Exploring Broader Implications
Understanding the entrainment of the entorhinal cortex provides a crucial central nervous system perspective that complements my understanding of the influenced peripheral vestibular system in MdDS. It suggests that the persistent illusion of motion is not solely a result of miscalibrated inner ear signals but also involves altered rhythmic activity within key brain regions responsible for spatial processing and sensory integration. This concept of entrainment, where an external rhythm can influence the brain's internal oscillations, has implications beyond MdDS.
Consider conditions like tics or Tourette's Syndrome. While the exact neurobiological mechanisms are complex and involve various brain regions, abnormal rhythmic activity and a tendency for neural circuits to fall into repetitive patterns are central to their manifestation. Specific internal or external triggers in susceptible individuals could lead to an entrainment-like process in motor control areas or the basal ganglia, resulting in the characteristic involuntary movements or vocalizations. While the specific brain regions and triggers differ significantly from MdDS, the underlying principle of rhythmic activity influencing neural circuits might share some conceptual similarities.
Beyond 'Sea Legs': When Adaptation Goes Awry
You might have heard the term ‘getting your sea legs,’ which describes how people who spend time on boats adapt to the constant motion. They become more attuned to the movement and develop strategies to maintain balance. This is a natural process of habituation and adaptation within the vestibular system.
However, this differs from conditions like Mal de Debarquement Syndrome (MdDS). While MdDS can sometimes be triggered by motion like being on a boat, the key difference lies in the individual's awareness and the nature of the adaptation:
'Sea Legs' - Conscious Adaptation: Individuals getting their sea legs are typically aware of the boat's motion. Their bodies and brains are actively learning to compensate for the predictable movements. They develop motor strategies, and their sensory systems recalibrate in response to the external motion. This adaptation usually resolves relatively quickly once they are back on stable ground.
MdDS - The Uninvited Guest: MdDS often develops subtly and can persist long after the motion stimulus has ceased. Individuals with MdDS usually experience a persistent sensation of rocking, swaying, or bobbing, even on stable ground. Unlike the conscious adaptation of getting sea legs, the mechanisms behind MdDS are not fully understood. Still, they are thought to involve a maladaptive response of the brain to motion, where the sensation of movement continues even in the absence of it. It can feel ‘sneaky’ because the onset might not be clearly tied to a specific event, or the individual might not initially recognize it as an abnormal persistence of motion sensation.
The key takeaway is that while the vestibular system is incredibly adaptable, sometimes this adaptation can become persistent and problematic, as seen in MdDS. Understanding this difference is crucial for both clinicians and individuals experiencing these symptoms.
In the context of MdDS, this holistic view reinforces the rationale behind our comprehensive vestibular rehabilitation approach. By strategically using controlled visual input to recalibrate vestibular reflexes and potentially disrupt maladaptive entrainment within the entorhinal cortex, we aim to provide more effective and long-lasting relief for individuals suffering from the often-debilitating symptoms of Mal de Debarquement Syndrome, guiding them back towards a stable and balanced life. Further research into the role of entrainment in various neurological conditions could unlock new avenues for understanding and treating a range of rhythmic and repetitive behaviors and perceptions.
References
[1] Kandel ER, Schwartz JH, Jessell TM, Siegelbaum SA, Hudspeth AJ. Principles of Neural Science. Fifth edition. New York, N.Y.: McGraw-Hill Education LLC., 2013.
[2] Dai M, Cohen B, Smouha E, Cho C. Readaptation of the vestibulo-ocular reflex relieves the mal de débarquement syndrome. Front Neurol. 2014;5:124. Published 2014 Jul 15. doi:10.3389/fneur.2014.00124
[3] Dai M, Cohen B, Cho C, Shin S, Yakushin SB. Treatment of the Mal de Debarquement Syndrome: A 1-Year Follow-up. Front Neurol. 2017;8:175. Published 2017 May 5. doi:10.3389/fneur.2017.00175
[4] Cha YH, Chakrapani S, Craig A, Baloh RW. Metabolic and functional connectivity changes in mal de debarquement syndrome. PLoS One. 2012;7(11):e49560. doi:10.1371/journal.pone.0049560
[5] Shou G, Yuan H, Urbano D, Cha YH, Ding L. Changes of symptom and EEG in mal de débarquement syndrome patients after repetitive transcranial magnetic stimulation over bilateral prefrontal cortex: a pilot study. Annu Int Conf IEEE Eng Med Biol Soc. 2014;2014:4294-4297. doi:10.1109/EMBC.2014.6944574
[6] Yuan H, Shou G, Gleghorn D, Ding L, Cha YH. Resting State Functional Connectivity Signature of Treatment Effects of Repetitive Transcranial Magnetic Stimulation in Mal de débarquement Syndrome. Brain Connect. 2017;7(9):617-626. doi:10.1089/brain.2017.0514
[7] Dupret D, Csicsvari J. The medial entorhinal cortex keeps Up. Nat Neurosci. 2012;15(11):1471-1472. doi:10.1038/nn.3245



