The Subtle Torsion of Horizontal Canal BPPV: A Critical Observation for Vestibular Professionals

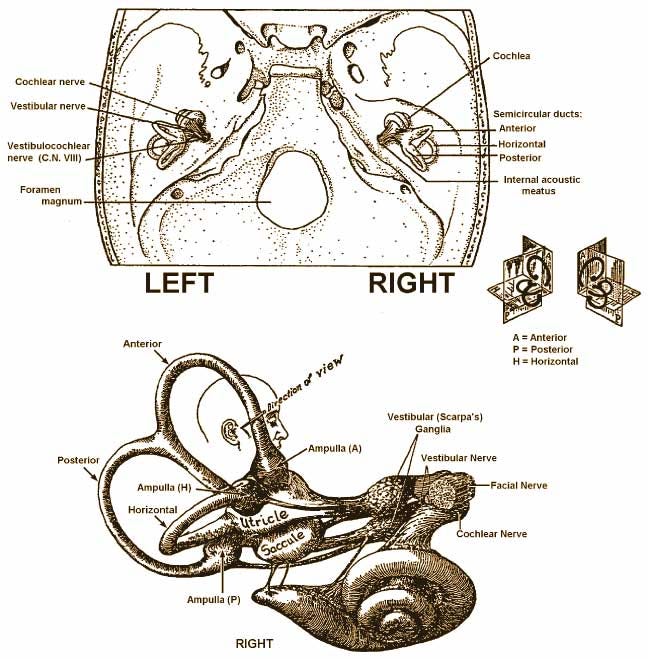
Benign paroxysmal positional vertigo (BPPV) involving the horizontal semicircular canal presents unique diagnostic challenges due to a frequently overlooked anatomical feature: the canal's inherent tilt. While often described as "horizontal," this canal deviates approximately 30 degrees from the horizontal plane, aligning more with Reid's line. This seemingly minor angulation has significant implications for the observed nystagmus and, consequently, for accurate diagnosis and effective treatment.
The Crucial Role of the 30-Degree Tilt in Diagnosing Horizontal Canal BPPV
Image: Johns Hopkins University - Max Brodell 1934
During positional testing, such as the supine roll test, the 30-degree tilt of the horizontal canal introduces a torsional component to the endolymph flow. This results in a nystagmus that is not purely horizontal, as might be expected, but instead exhibits a torsional subtle element. While often easily missed without careful observation, this subtle torsion is a crucial differentiator from the more pronounced torsional nystagmus seen in vertical canal BPPV. Understanding this clinical implication is vital for accurate diagnosis and effective treatment of horizontal canal BPPV.
Distinguishing Horizontal from Vertical Canal BPPV
Video: Upbeat & Torsion in the PSC-BPPV Patient
The torsional nystagmus observed in the horizontal canal BPPV is distinct from that seen in the posterior and anterior canal BPPV. In vertical canal BPPV, the nystagmus presents as a dominant upbeat or downbeat component with an accompanying torsion. In contrast, horizontal canal BPPV exhibits a predominantly horizontal nystagmus with a subtle torsional overlay.
Video: Right beating with a possible subtle torsion of an HSC-BPPV.
2 Videos: Left beating with a possible subtle torsion of an HSC-BPPV.
Clinical Significance
Recognizing this subtle torsion is crucial for several reasons:
Accurate Diagnosis: Differentiating horizontal canal BPPV from other forms of BPPV, including those affecting the vertical canals, ensures the selection of the appropriate canalith repositioning maneuver.
Targeted Treatment: Misinterpreting the nystagmus can lead to ineffective treatment or even worsening symptoms. Precise identification of the affected canal guides the clinician in applying the correct repositioning technique.
Improved Patient Outcomes: Accurate diagnosis and targeted treatment lead to faster symptom resolution, minimizing patient discomfort and maximizing the effectiveness of vestibular rehabilitation.
Enhancing Observational Skills
Vestibular professionals are encouraged to refine their observational skills to discern the subtle torsion in horizontal canal BPPV. Utilizing infrared video goggles during positional testing can enhance visualization of eye movements, aiding in detecting this often-overlooked characteristic.
Supporting Evidence
While dedicated research quantifying the torsional component in horizontal canal BPPV is limited, the anatomical basis for this phenomenon is well-established. Anatomical studies consistently demonstrate the horizontal canal's 30-degree angulation. Furthermore, clinical experience and expert consensus support the presence of subtle torsion in horizontal canal BPPV.
Conclusion
The subtle torsion associated with horizontal canal BPPV is critical for vestibular professionals. By recognizing this nuanced feature, clinicians can ensure accurate diagnosis, implement targeted treatment strategies, and optimize patient outcomes. Continued emphasis on meticulous observation and a thorough understanding of the vestibular system's anatomical intricacies is essential for advancing the care of individuals with BPPV.


Thanks for another great article Brian! So helpful to see those eye movement videos!
Very timely article, I saw this today in clinic. Thank you for your contribution to the vestibular community