The Vestibular Catastrophe: Ozempic, Mounjaro, and the Destruction of Balance and Sensory Systems

We must confront the most severe pharmacological threat to the vestibular system in a generation. We face an undeniable clinical crisis, supported by 496,756 patient records. This study confirms that the widespread use of GLP-1 receptor agonists (GLP-1RAs)—Ozempic (Semaglutide), Mounjaro (Tirzepatide), and related drugs like Wegovy—is a direct catalyst for organ destruction and systemic microvascular failure. We look at a catastrophe spanning the inner ear, the cochlea, and the retinal macula.
The Methodological Authority: The Uncut Truth of 496,756 Patient Records
The scale of this investigation lends it an overwhelming, final authority. The researchers used the TriNetX research network to analyze outcomes for 496,756 patients who initiated GLP-1RA therapy.
The rigor of this study defeats common counter-arguments. Researchers employed Propensity Score Matching to rigorously control for all known confounders, including diabetes, obesity, and hypertension. The conclusion is inescapable:
The risk is independent. The drug itself drives the destruction.
Defining the Threat: What the Hazard Ratio Really Means
The Hazard Ratio (HR) is the most crucial statistic in this study. It is simply a risk multiplier.
When the study reports an HR of 4.95 for Semaglutide, it means:
The group taking Ozempic is running the race toward a vestibular diagnosis almost five times faster than the group not taking the drug. They are 495% more likely to be diagnosed with a balance disorder at any point in time.
🚨 The Uncut Statistical Reality: The Raw Data
Ozempic (Semaglutide) HR at 3 years: 4.95 (95% CI: 4.51–5.43). The risk approaches five times the background rate in the long term.
Mounjaro (Tirzepatide) HR at 3 years: 4.55 (95% CI: 3.43–6.03). This drug also carries a risk nearly 4.5 times the background rate.
Risk Ratio (RR) at 3 years: 2.04. Comparing Semaglutide to Tirzepatide, this shows that Ozempic/Wegovy carries twice the long-term risk of Mounjaro/Zepbound.
Pathology of Organ Destruction: Systemic Catastrophe
We must identify BPPV for what it truly is: the hallmark of Utricular Macular Degeneration. The pathology is systemic and destructive, focusing on three vital sensory systems:
1. Otolithic Destruction and Central VNC Corruption
The medication causes the otoconia to shed because the macula is failing. This is the physical destruction of the otolithic bed. It obliterates the patient’s gravity receptor, leading to chronic instability. Furthermore, the drug actively crosses the Blood-Brain Barrier (BBB), disrupting the Vestibular Nuclei Complex (VNC), thereby destroying the brain’s ability to establish a stable compensatory baseline.
2. Microvascular Catastrophe: Cochlea and Retina
The GLP-1RA mechanism is one of vasodilation and metabolic stress that attacks shared, sensitive microcirculations:
Inner Ear and Cochlea: The drug’s vasodilation perturbs pressure and fluid homeostasis in the inner ear via the ‘stria vascularis’. This creates Meniere‘s-like symptoms and compromises the hair cells within the ‘Organ of Corti’. The stria vascularis maintains the high positive Endolymphatic Potential ($EP$); by compromising this structure, the drug causes an endolymphatic hydrops, severely disrupting the electrical environment necessary for sensory transduction.
Retinal Macula (Visual System): Patient complaints of visual darkness and hypoperfusion point to a real risk of ‘retinal vascular insufficiency’ in the highly metabolic macula of the eye.
The Clinical Smoking Gun: A Case Study in Iatrogenic Catastrophe
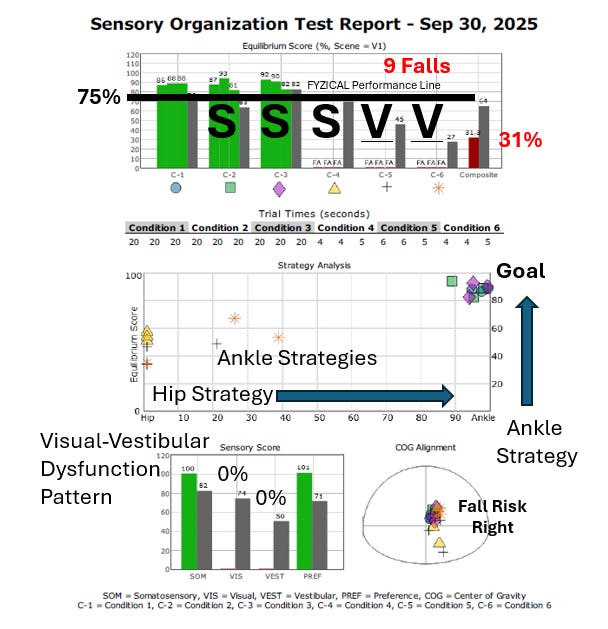
The objective findings from a patient on Ozempic confirm the pathology predicted by the statistical cohort. This patient’s Dizziness Handicap Inventory (DHI) score—a measure of perceived functional, emotional, and physical difficulty—was a catastrophic 78 points. SOT testing (see below) showed a profound vestibular dysfunction pattern defined as a SVVM (Somatosensory > Visual-Vestibular Mismatch). This means that, because the vestibular system is not responding, the brain is relying more on her feet and eyes for sensory input, leading to persistent dizziness.
Furthermore, testing provoked a profound Downbeat Nystagmus, confirming Central Vestibular System (VNC) corruption by the drug. The patient’s eventual relapse upon restarting Ozempic proves the drug is the pathological driver, perpetually compromising the VNC and preventing therapeutic gain.
The Mandate: Future Research and Clinical Protocols
The disease process starts immediately. We must leverage this data to institute new clinical and research mandates.
Pharmacological Vestibulotoxicity and Genetic Susceptibility
We must stop treating this as an anomaly; we recognize this as Pharmacological Vestibulotoxicity. Future research must immediately address the question of genetic susceptibility. The field needs to identify specific genetic markers governing GLP-1 receptor expression—both in the central VNC and in the peripheral vascular regulatory pathways. Finding these genes enables us to develop screening tools to identify high-risk patients before a prescription is ever written, preventing permanent destruction of their otolithic systems. This is the only ethical path forward.
Advanced Objective Monitoring
We must push for standardized objective testing protocols in prospective trials. We need studies utilizing:
Video Head Impulse Test (vHIT) and Vestibular Evoked Myogenic Potentials (VEMPs) to precisely quantify the otolithic and semicircular canal damage.
Serial Testing during dose escalation to determine the chemical tipping point for the VNC.
The Clinical Protocol
The vestibular professional now holds the key prognostic data. Our role is to aggressively rehabilitate the system to compensate for the permanent damage done to their otolithic organs. We must frame BPPV as evidence of Macular Degeneration, and we must inform prescribing physicians that continuous GLP-1RA exposure compromises the patient’s capacity for neuroplasticity. The permanent nature of the otolithic loss means these patients require long-term management against profound dependency strategies like SVVM and VSVM.
Brian Werner, PT, MPT, is a physical therapist who has been specializing in vestibular and balance disorders for over a quarter of a century. He is the founder of the FYZICAL Balance Paradigm and one of the co-founders of FYZICAL, LLC, Balance Center Division with Dr. Daniel Deems, MD, PhD, where he serves as the National Director of Vestibular Education & Training.
References
Toraih, E. A., Alenezy, A., Hussein, M. H., Hashmat, S., Mummadi, S., Alrawili, N. F., Abdelmaksoud, A., & Fawzy, M. S. (2025). The Risk of Vestibular Disorders with Semaglutide and Tirzepatide: Findings from a Large Real-World Cohort. Biomedicines, 13(5), 1049.


We just discussed this as a clinic, and , as therapists who work in the CNS and with visceral connections to musculoskeletal disorders, we are concerned. We are redoubling efforts to discuss nutrition, exercise and a more healthy lifestyle with our patients, but understanding people are being offered a quick fix, and they are more likely to take that route. We will be needed more than ever in the near future.
I agree. The challenge is they likely won't know until they get older or blame it on something else.