Unmasking WEBINO: The "Wall-Eyed" Gaze That Demands Attention

As a physical therapist specializing in vestibular and balance disorders, I've encountered numerous neurological presentations as the National Director of Vestibular Education & Training at FYZICAL. However, a few conditions are visually striking and crucial to comprehend, such as wall-eye bilateral internuclear ophthalmoplegia (WEBINO).
This condition, which causes the eyes to turn outward, creating a 'wall-eyed' appearance, is a profound indicator of significant brainstem activity. Understanding WEBINO is not just an academic exercise; it's a critical aspect of our role in patient care, particularly in rehabilitation and balance, where identifying the root cause of disequilibrium and visual disturbances is paramount.
As a physical therapist, your understanding of these complex neurological deficits is not just important; it's paramount. Your role in rehabilitation, especially for balance, often hinges on recognizing the root cause of disequilibrium and visual disturbances. WEBINO is a perfect example of a condition where your keen observation can lead to a timely diagnosis and, hopefully, better patient outcomes.
What is WEBINO? The Gaze That Gives It Away
At its core, WEBINO is a rare but distinct ocular motility disorder. Imagine trying to look inwards towards your nose. With WEBINO, both eyes struggle or fail to move inward (bilateral adduction deficit).
When the eyes attempt to move outward, you'll often see rapid, involuntary jerking movements, known as abducting nystagmus. The most striking feature, however, is the large-angle exotropia in primary gaze, meaning that when the patient looks straight ahead, both eyes deviate outward, giving them that characteristic "wall-eyed" look. Difficulty focusing on near objects (impaired convergence) is also an everyday companion to these signs.
The Brain's Crossroads: Where WEBINO Takes Root
The eyes are the windows to the soul, but in WEBINO, they are also a window to the brainstem. The culprit behind WEBINO is typically a lesion or damage to a crucial neurological pathway called the medial longitudinal fasciculus (MLF), specifically on both sides.

Think of the MLF as a high-speed data cable connecting the parts of your brain that coordinate eye movements. It links the abducens nucleus (which helps your eye move outward) with the oculomotor nucleus (which helps your eye move inward) on the opposite side. When both "cables" are damaged, the communication breaks down, leading to WEBINO's characteristic eye movement abnormalities. The outward deviation (exotropia) itself is likely to arise from this disruption due to the involvement of specific subnuclei or an imbalance in other eye movement centers.
The Underlying Whys: What Causes WEBINO?
Understanding WEBINO's underlying cause is critical, as treatment hinges on addressing the primary problem. While less common, these are some of the key culprits:
Cerebrovascular events (Stroke): This is a common cause, especially in older individuals. A lack of blood flow (ischemia) to the brainstem can damage the MLF.
Multiple Sclerosis (MS): In younger patients, MS is a frequent cause. The demyelination (damage to the protective sheath around nerve fibers) typical of MS can affect the MLF bilaterally.
Neurodegenerative disorders: Conditions like Progressive Supranuclear Palsy (PSP) can also lead to WEBINO.
Infections: Various bacterial, viral, or fungal infections, including meningoencephalitis, can inflame or damage the brainstem.
Inflammatory conditions: Sarcoidosis, lupus, and Behçet disease are examples.
Trauma: Head injuries can, in rare cases, impact the brainstem.
Tumors: Growths in or near the brainstem can compress or destroy the MLF.
Nutritional deficiencies: Conditions like Wernicke's encephalopathy.
Drug toxicity: Certain medications can rarely have this as a side effect.
Congenital malformations, Such as Arnold-Chiari malformation.
The Diagnostic Journey: Pinpointing the Problem
Diagnosing WEBINO relies on a combination of careful observation and advanced imaging:
Clinical Examination: As physical therapists, our detailed observation of eye movements is crucial. We look for those tell-tale signs: the bilateral inability to adduct, the abducting nystagmus, and the "wall-eyed" appearance.
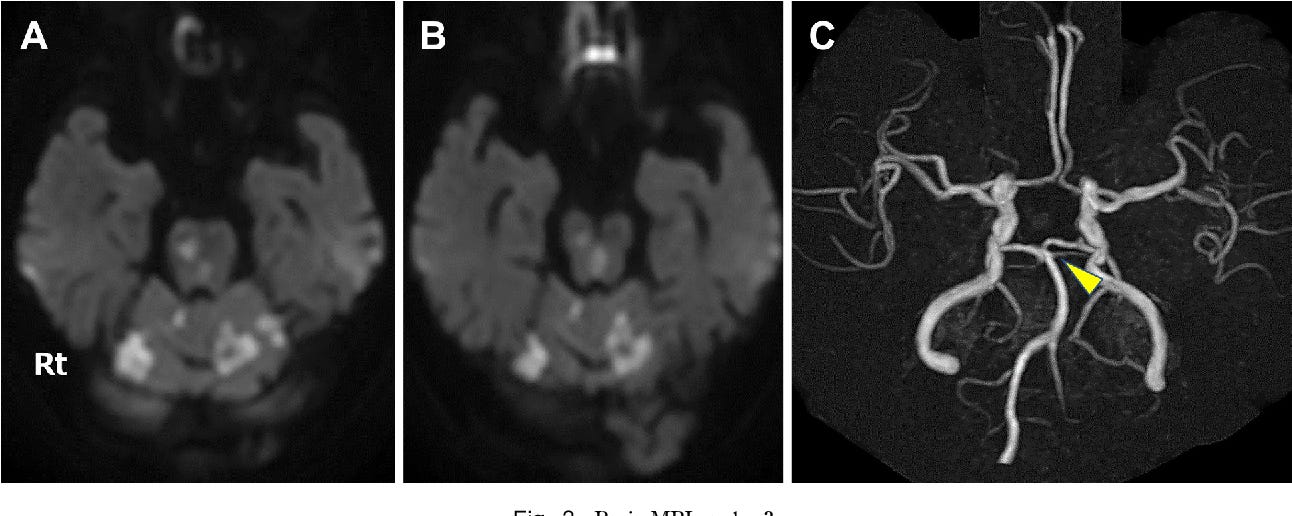
Brain MRI: This is the gold standard for identifying the underlying lesion. MRI of the brain, particularly sequences like T2-weighted and FLAIR, can pinpoint damage in the brainstem (pons or midbrain). Diffusion-weighted imaging (DWI) is beneficial for detecting acute strokes.
Further Investigations: Depending on the suspected cause, blood tests or cerebrospinal fluid (CSF) analysis might be ordered to rule out infections, inflammatory conditions, or specific demyelinating diseases like Neuromyelitis Optica Spectrum Disorder (NMOSD).
Treatment and Prognosis: A Path Towards Recovery (or Adaptation)
The immediate focus of therapy for WEBINO is always on addressing the underlying cause.
If it's a stroke, acute stroke management and secondary prevention strategies (like antiplatelet medications) are critical.
For MS or NMOSD, immunomodulatory therapies are used to manage the disease.
The medical team would treat infections, tumors, or nutritional deficiencies accordingly.
Beyond treating the cause, managing the symptoms, particularly double vision (diplopia) and misalignment of the eyes (strabismus), is essential. This can involve:
Corrective lenses: Often with prism lenses to help merge the images.
Botox injections: Injected into specific eye muscles to reduce misalignment.
Extraocular muscle surgery: For stable, long-standing exotropia.
Neuro-optometric rehabilitation: This is where our expertise truly shines! A systematic approach can help patients improve oculomotor function, range of motion, and overall visual comfort. While we don't treat the WEBINO, we can help patients adapt and maximize their remaining visual function and balance control. This is particularly important for patients with profound vestibular dysfunction who may rely heavily on visual cues (VSVM) or surface cues (SVVM).
The prognosis for WEBINO varies significantly depending on what caused it. Cases due to demyelination, infections, or trauma tend to have a better chance of full recovery. However, if it's caused by a large stroke or a progressive neurodegenerative disease, the recovery may be limited. About half of all INO (Internuclear Ophthalmoplegia) cases, including WEBINO, resolve within a year, offering hope for patient recovery.
The "Substack" Takeaway: Why This Matters to Us
As physical therapists specializing in balance, recognizing the nuanced signs of conditions like WEBINO isn't just academic; it directly impacts our assessment and intervention strategies. A patient presenting with dizziness, imbalance, and those tell-tale 'wall-eyes' isn't just someone with a balance problem; they're someone who needs immediate neurological attention. This is where collaboration with neurologists becomes essential, reinforcing the significance of our professional relationships.
Our understanding helps us:
Screen effectively: Knowing what to look for allows us to identify red flags and ensure timely medical referrals.
Collaborate better: We can communicate more effectively with neurologists and other healthcare professionals.
Tailor rehabilitation: While the underlying lesion may not be reversible by therapy, we can address the resulting functional deficits, improve gaze stability, and implement sensory strategies. For example, suppose a patient is struggling with Visual-Vestibular Mismatch (VVM) or Somatosensory-Vestibular Mismatch (SVM) due to their profound vestibular challenges from the brainstem lesion. In that case, our interventions can focus on integrating remaining sensory inputs and teaching compensatory strategies. We could use our Safety Overhead Support (SOS) System exclusively at FYZICAL Therapy & Balance Center to challenge balance safely.
WEBINO is a powerful reminder that the eyes are inextricably linked to the brain, and profound changes in eye movement can signal significant neurological compromise. By staying informed and acutely observant, we, as physical Therapists, can play a pivotal role in the journey of these unique and often challenging patients.


