Unraveling the Nuances of Posterior Canal BPPV: A Deeper Dive into Heavy Cupula Diagnostics

Brian Werner, PT, is back with you for another exploration into the fascinating world of vestibular disorders.
This week, I want to delve deeper into a crucial aspect of diagnosing Benign Paroxysmal Positional Vertigo (BPPV), specifically concerning the "graviceptive heavy posterior canal cupula." As vestibular therapists, we strive for precise diagnoses to ensure effective treatment, and a recent case series offers some compelling insights into differentiating the underlying causes of this particular presentation.
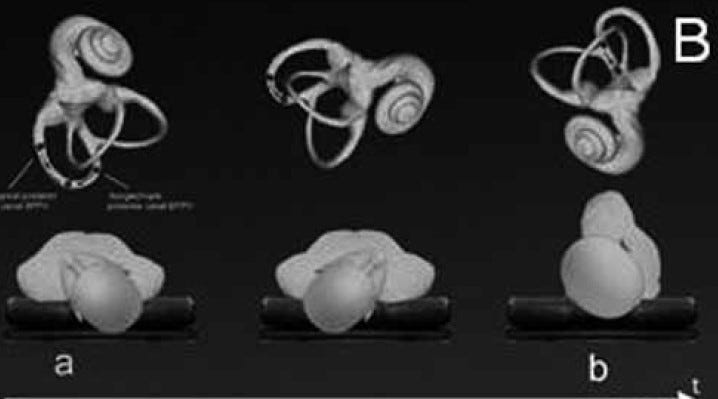
The study I'm referring to, 'Inversion Test and Sitting-Up Oculomotor Patterns in Patients with Graviceptive Heavy Posterior Cupula – A Case Series' by Vats et al., published in the Journal of International Advanced Otology in 2024, is a significant contribution to our understanding of BPPV. It examined the subtle yet important differences between two conditions that can lead to a posterior semicircular canal (PSC) cupula becoming heavy and gravity-sensitive: posterior cupulolithiasis and a specific type of canalithiasis.
Recap of the Study
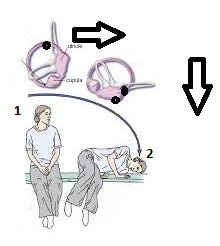
The researchers investigated nine patients exhibiting symptoms consistent with a heavy posterior cupula, characterized by prolonged upbeating and torsional nystagmus during the Half-Hallpike Test (HHT). They aimed to understand the diagnostic oculomotor patterns better and to propose a grading system for an inversion test that could distinguish between:
Posterior Cupulolithiasis (PSC-BPPV-cu): Where otoconia adhere directly to the cupula.
Short-Arm Posterior Semicircular Canalolithiasis (PSC-BPPV-sa): Where free-floating otoconia in the short arm of the PSC fall onto the utricular side of the cupula upon sitting up, effectively weighting it down.
Decoding the Inversion Test: Understanding the "Why" Behind the Nystagmus
The beauty of the inversion test lies in understanding the mechanics of how gravity and the otoconia interact with the cupula in each of these conditions. Here's a more detailed explanation of what's happening:
When you perform the Half-Hallpike Test on a patient with a heavy posterior cupula, you essentially bring the affected posterior semicircular canal into a gravity-dependent position.
This causes the heavy cupula to deflect, leading to the characteristic upbeating and ipsitorsional nystagmus. This would be:
Right PSC-BPPV-cupulo = Upbeating Torsion to the Right
Left PSC-BPPV-cupulo = Upbeating Torsion to the Left
The inversion test then shows that in cupulolithiasis, the otoconia are stuck to the cupula, whereas in the short-arm canalithiasis, they are free to move.
A. Strongly Positive Inversion Test (PSC-BPPV-cupulo): The otoconia firmly adhere to the cupula in this scenario. When you move the patient into the contralateral recumbent, nose-down position (the inversion position), the direction of gravity's pull on the cupula reverses. Since the otoconia are still attached, they continue to weigh down the cupula, causing it to deflect in the opposite direction. This results in a downbeating and contratorsional nystagmus that is often just as intense as the initial upbeating nystagmus. This would be:
Right PSC-BPPV-cupulo = Downbeating Torsion to the Left
Left PSC-BPPV-cupulo = Downbeating Torsion to the Right
Think of it like a weight stuck on a pendulum – when you swing it one way, the weight makes it go, and when you swing it the other way, the weight still influences its movement in the opposite direction.
B. Weakly Positive Inversion Test (Coexistence): A weakly positive result suggests a mixed picture. Some otoconia might be adhered to the cupula (contributing to the downbeating nystagmus in the inversion test), while others are free-floating in the short arm (leading to a less intense response than pure cupulolithiasis). This indicates that the cupula is only partially "off-loaded" in the inverted position, as some particles remain attached.
C. Negative Inversion Test (PSC-BPPV-short arm): The otoconia do not adhere to the cupula. They are sitting on the utricular side, making the cupula heavy in certain positions, like when the patient is brought into the HHT position or when they sit up. However, when you move the patient into the inversion position (contralateral recumbent, nose down), gravity now pulls the free-floating otoconia away from the utricular side of the cupula and back into the short arm of the posterior semicircular canal. With the weight removed from the cupula, it returns to its resting position, and the nystagmus disappears. It's like having sandbags temporarily placed on a lever – when you flip the lever, the sandbags fall off, and the lever no longer moves oppositely.
Clinical Implications for Practitioners
Understanding these biomechanical principles is paramount for us as practitioners. The study's findings can guide us in recognizing the nystagmus reversal with a vigorous intensity in the inversion test, which strongly points towards cupulolithiasis. This understanding could initially guide us towards specific liberatory maneuvers or aggressive habituation exercises. Conversely, a negative inversion test, coupled with nystagmus on sitting up, strongly suggests short-arm canalithiasis, which might respond well to specific positioning strategies or the home-based Brandt-Daroff exercises as highlighted in the study.
Observing anteroposterior truncal oscillations (i.e, pseudo-Tumarlin-Like phenomenon) when sitting up in some PSC-BPPV-sa cases also provides an important clinical clue. This suggests a more significant impact of the otoconial debris on the vestibular system in this specific presentation.
Treatment Strategies Beyond Brandt-Daroff
The study found that while initial treatment with standard maneuvers didn't provide immediate relief, all nine patients eventually became asymptomatic after four weeks of home-based Brandt-Daroff exercises. However, it's important to remember that vestibular rehabilitation offers a range of techniques for addressing a heavy posterior cupula. Beyond Brandt-Daroff exercises, several manual maneuvers aim to resolve this specific type of BPPV:
Califano Maneuver: This maneuver involves quickly rolling the patient into a nose-down position from the Dix-Hallpike position. The rapid movement is theorized to create a pushing force that dislodges otoconia adhered to the cupula. This could be repeated back and forth, creating what might be described as a lying-down BASTORE Maneuver.
Half-Semont Technique: Starting with the patient sitting, this technique involves quickly moving the patient into a side-lying position with the affected ear up, similar to the Semont maneuver but with a less extensive initial positioning. The rapid change in gravity is thought to generate a pushing effect on debris in the posterior canal's short arm.
BASTORE ( Bi-directional Arm Semont Therapy with Opposite Repositioning Exercise) Maneuver: This technique begins with the patient in a nose-down position. They are then quickly brought up to sitting, which is hypothesized to create a pulling force, drawing the cupula away from any adhered debris. If symptoms persist, the patient is moved back into the side-lying position (as in the Semont maneuver) on the initially tested side, then returned to the nose-down starting position. This repetitive pushing and pulling action aims to dislodge the otoconia from the cupula.
In Conclusion
The 2024 study by Vats et al. provides valuable insights into the nuances of the graviceptive heavy posterior cupula. By understanding the mechanisms behind the inversion test results and carefully observing oculomotor patterns, we, as vestibular practitioners, can refine our diagnostic skills and tailor our treatment approaches for patients with these specific presentations of posterior canal BPPV. This knowledge empowers us to provide even more effective and targeted care.
What are your experiences with these different presentations of posterior canal BPPV? Have you utilized an inversion test in your practice? Your thoughts and insights are valuable to our community. Please share them in the comments below!
Reference
Vats AK, Kothari S, Khamesra R, Vats S. Inversion Test and Sitting-Up Oculomotor Patterns in Patients with Graviceptive Heavy Posterior Cupula - A Case Series. Ann Indian Acad Neurol. 2023 Sep-Oct;26(5):769-773. doi: 10.4103/aian.aian_379_23. Epub 2023 Oct 7. PMID: 38022454; PMCID: PMC10666849.